Best Lung Cancer Treatment in the USA
Lung Cancer Treatment
Healthiza Lifescience is committed to sharing clear, up -to -date information, so that patients and families can take confident decisions. In the United States, lung cancer has become a major cause of cancer death for both men and women, but the results are previously improving thanks to detection and modern treatments. As per the 2025 data, the National Cancer Institute estimates 226,650 new cases and 124,730 deaths from lungs and bronchus cancer, with an existence of 5 years relative to 28.1% -a number that increases in the form of advances of care. In the last decade, the mortality rate is falling about 4% per year, an indication that screening and better treatment are saving lives.
Why Early Detection Matters
Detecting lung cancer early is the most powerful way to improve existence. When the disease is found in a local stage, the 5 -year survival rate is about 64.7%; Once it spreads from a distance, it falls to ~ 9.7%. Unfortunately, more than half of cases are still diagnosed after cancer is already metastasized, which is why screening is important.
Who Should Get Screened?
Two major guidelines inform US screening:
USPSTF (U.S. Preventive Services Task Force): The annual low-dose CT (LDCT) for adults 50-80 with 20 pack-year history that currently smokes or leaves within the last 15 years; Smoking free after 15 years or if a person can’t undergo therapeutic treatment.
American Cancer Society (2023 update): annual LDCT for adults 50–80 with ≥20 pack-years who currently smoke or smoked in the past, without a 15-year quit-time limit. This expands eligibility to many long-time quitters who still take high risk.
Talk with your doctor which guidelines apply to you, potential benefits (earlier detection) and harms (false positive, casual conclusions), and how to quit smoking if you still use tobacco.
Understanding the Types of Lung Cancer
Treatment plans depend on the type and stage:
- Non-Small Cell Lung Cancer (NSCLC) (~ 85% cases): Adenocarcinoma, squamous cell carcinoma and large cell carcinoma are included.
- Small cell lung cancer (SCLC) (~ ~ 15%): increases and spreads rapidly and is usually treated differently.
What is the Best Lung Cancer Treatment?
There is no “best” therapy for every patient. The optimal plan is individual -built as per stage, tumor genetics (biomarker), overall health and patient preferences. It is mentioned here how state -of -the -art care is seen in 2025.
Surgery & Radiation for Initial Stage Disease
For the initial stage NSCLC, surgery (depending on the size and location of the lobectomy or segmentectomy) provides the highest chance of treatment. When surgery is not possible, stereotactic body radiotherapy (SBRT) may accurately radiate for tumors. Some patients benefit from therapy (after surgery) or neoadjuvant (before surgery) to reduce repetitive risk.
Chemoradiation & Consolidation
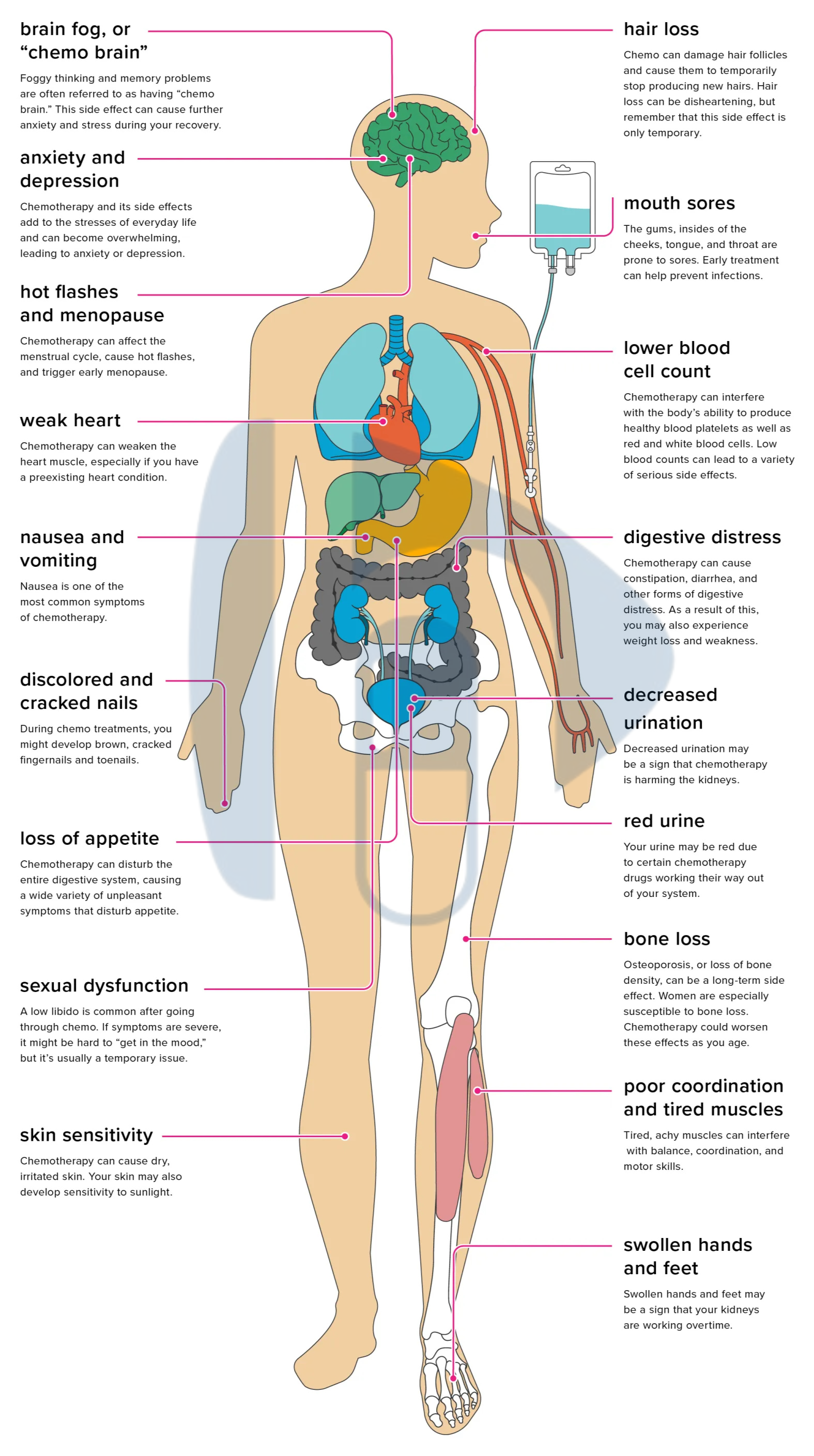
Locally advanced (usually phase III) for NSCLC that cannot be surgically removed, combined chemotherapy plus radiation is effective. Many patients receive a consolidation immunotherapy to help control cancer.
Targeted Therapy
A cornerstone of modern Lung Cancer care is comprehensive molecular test on tissues (or even blood). If your cancer harbors a driver mutation – such as EGFR, ALK, ROS1, Braf, MET, RET, NTRK, or Kras G12C – You can be eligible for an oral targeted therapy that often works with better and less side effects than traditional chemotherapy for that mutation. These drugs can be used in metastatic disease and, for some mutation (eg, EGFR), after surgery for repetition risk cuts.
Immunotherapy
Immune checkpoint inhibitors (such as PD -1/PD -L1 blockers) have resumed treatment for many patients with advanced NSCLC and are also used in some stage 3 cases even after chemoradiation. They help the immune system identify and attack cancer cells and can give sustainable reactions in patients.
Small Cell Lung Cancer Breakthroughs
SCLC is highly sensitive to chemoradiation, but relapses are common. A major 2024 advance: FDA approved the Durvalumab as a consolidation therapy after concurrent chemoradiation for limited-phase SCLC based on phase 3 adsriatic testing-a new standard of first approved immunotherapy and care for this stage.
Build a Personal Treatment Plan
A top level American cancer center will usually be:
- When indicated, CT, PET/CT, and brain MRI done accurately.
- Testing comprehensively: PD-L1 and next generation sequencing for target mutation in NSCLC; Imaging and laboratory suitable for SCLC.
- Present your case to the tumor board so that surgeons, medical oncologists, radiation oncologists, pulmonologists and pathologists weigh together.
- Sequence therapy: Surgery ‘Neoadjuvant/adjuvant therapy, or definitive chemoradiation with immunotherapy, or targeted therapy first for driver-positive disease.
- Support you with a holistic manner with smoking, nutrition, pulmonary rehabilitation and side-effect management.
These phases align with the guidance of the National Cancer Institute that standard treatment options include surgery, radiation therapy, chemotherapy, targeted therapy and immunotherapy, which are individual to the tumour type and phase.
Risk Reduction Still Matters
While treatment has improved, prevention saves the most life. Smoking drives most cases of lung cancer; Leaving smoking reduces the risk over time, and the screening helps in catching cancer as soon as possible. There is also a low risk for avoiding radon mitigation and commercial carcinogenes at home. If you qualify for LDCT, discuss it with your doctor – especially if you are between 50 and 80 with heavy smoking history.
What to Ask your Care Team
- Do I qualify for LDCT screening under ACS or USPSTF criteria?
- What stages and type of lung cancer do I have?
- Has my tumor biomarker-testing? If positive, what targeted options exist?
- Should I consider immunotherapy after now or after radiation?
- Am I eligible for a clinical test?
- Can supporting care services help me stay strong during treatment?
Healthiza Lifescience Commitment
In Healthiza Lifescience, we believe that every person facing lung cancer is entitled to a treatment plan and conforms to their goals. From education to access support, our team partners with clinicians and patients to navigate choices – whether it is surgery, SBRT, targeted therapy, chemicals, or immunotherapy. If a new diagnosis is made to you or a loved one, ask about comprehensive testing and multi-disciplinary reviews. Better knowledge leads to better care.
Disclaimer: This article is educational and not an alternative to medical advice. Always consult your healthcare provider for diagnosis and treatment decisions.
Source: American Cancer Society, National Cancer Institute SEER and PDQ, USPSTF, and 2024-2025 updated on Durvalumab for Limited SCLC,
Also Read,









 Bevacizumab Injection is a cancer-fighting medicine. It’s used to treat colon and rectum cancers, as well as non-small cell lung cancer, kidney cancer, brain tumours, and ovarian and cervical cancers. It helps to halt tumour growth by preventing the creation of new blood vessels that feed tumours. When used with other cancer medications, bevacizumab Injection is an excellent first-line choice.
Bevacizumab Injection is a cancer-fighting medicine. It’s used to treat colon and rectum cancers, as well as non-small cell lung cancer, kidney cancer, brain tumours, and ovarian and cervical cancers. It helps to halt tumour growth by preventing the creation of new blood vessels that feed tumours. When used with other cancer medications, bevacizumab Injection is an excellent first-line choice.  Trastuzumab injection is a type of anticancer medicine that is used to treat some types of breast, stomach, and esophageal cancers. It is sometimes used in conjunction with other cancer drugs. This medicine is used to treat cancers that produce an excessive amount of a chemical known as HER2 protein. It is a drug that works by slowing or preventing the growth of cancer cells. It is occasionally used when cancer has spread to other places of the body.
Trastuzumab injection is a type of anticancer medicine that is used to treat some types of breast, stomach, and esophageal cancers. It is sometimes used in conjunction with other cancer drugs. This medicine is used to treat cancers that produce an excessive amount of a chemical known as HER2 protein. It is a drug that works by slowing or preventing the growth of cancer cells. It is occasionally used when cancer has spread to other places of the body.  Paclitaxel Injection is an effective anticancer medicine. It is used to treat Breast, Pancreatic, and non-small cell Lung cancer. This medication can be used alone or in conjunction with other drugs or treatments such as chemotherapy. It improves breast cancer symptoms such as breast lumps, bloody nipple discharge, and changes in the form or texture of the breast. Paclitaxel Injection destroys or slows the tumour growth while also preventing them from multiplying.
Paclitaxel Injection is an effective anticancer medicine. It is used to treat Breast, Pancreatic, and non-small cell Lung cancer. This medication can be used alone or in conjunction with other drugs or treatments such as chemotherapy. It improves breast cancer symptoms such as breast lumps, bloody nipple discharge, and changes in the form or texture of the breast. Paclitaxel Injection destroys or slows the tumour growth while also preventing them from multiplying.  Bortezomib injection is an anticancer medicine that is used to treat multiple myeloma and mantle-cell lymphoma. It works by preventing or decreasing protein degradation in cells. As a result, the number of proteins in cancer cells increases, leading to their elimination.
Bortezomib injection is an anticancer medicine that is used to treat multiple myeloma and mantle-cell lymphoma. It works by preventing or decreasing protein degradation in cells. As a result, the number of proteins in cancer cells increases, leading to their elimination.  Abiraterone Acetate Tablets are a cancer-fighting drug. It works by suppressing the generation of androgen (male hormone) in men to treat prostate cancer that has progressed to other parts of the body. It is prescribed for men who are unable to treat their prostate cancer with surgeries or other medications. Abiraterone acts by inhibiting the production of androgen in the body. Androgens are man hormones that can encourage prostate gland tumour growth.
Abiraterone Acetate Tablets are a cancer-fighting drug. It works by suppressing the generation of androgen (male hormone) in men to treat prostate cancer that has progressed to other parts of the body. It is prescribed for men who are unable to treat their prostate cancer with surgeries or other medications. Abiraterone acts by inhibiting the production of androgen in the body. Androgens are man hormones that can encourage prostate gland tumour growth.  Dasatinib tablet is used to treat blood cancer (chronic myeloid leukemia-CML, acute lymphoblastic leukemia-ALL). It is used in people whose condition has not responded to existing leukaemia medicines or who are unable to use these medications due to side effects. It works by stopping or preventing cancer cell proliferation.
Dasatinib tablet is used to treat blood cancer (chronic myeloid leukemia-CML, acute lymphoblastic leukemia-ALL). It is used in people whose condition has not responded to existing leukaemia medicines or who are unable to use these medications due to side effects. It works by stopping or preventing cancer cell proliferation.  It is used in the treatment of Breast cancer, Pancreatic cancer, Lung cancer and Kidney cancer. Moreover, it is also used to control the immune system during organ transplantation. A transplanted organ, such as a liver or kidney, can potentially be attacked or “rejected” by the immune system. Because the immune system considers the new organ as an invader. Everolimus tablet is used to keep organs from rejecting following a kidney or liver transplant. It controls the immune response of the body so that the new organ can be accepted.
It is used in the treatment of Breast cancer, Pancreatic cancer, Lung cancer and Kidney cancer. Moreover, it is also used to control the immune system during organ transplantation. A transplanted organ, such as a liver or kidney, can potentially be attacked or “rejected” by the immune system. Because the immune system considers the new organ as an invader. Everolimus tablet is used to keep organs from rejecting following a kidney or liver transplant. It controls the immune response of the body so that the new organ can be accepted.  Erlotinib tablet is used to cure certain types of non-small cell lung cancer that have progressed to neighbouring tissues in patients who have failed to respond to at least one other chemotherapy medicine. It is also used in conjunction with another drug “gemcitabine” to cure pancreatic cancer that has progressed to neighbouring tissues or other parts of the body and is resistant to surgery. It works by preventing cancer cells from multiplying by stopping the action of an aberrant protein. This slows or stops cancer cells from spreading.
Erlotinib tablet is used to cure certain types of non-small cell lung cancer that have progressed to neighbouring tissues in patients who have failed to respond to at least one other chemotherapy medicine. It is also used in conjunction with another drug “gemcitabine” to cure pancreatic cancer that has progressed to neighbouring tissues or other parts of the body and is resistant to surgery. It works by preventing cancer cells from multiplying by stopping the action of an aberrant protein. This slows or stops cancer cells from spreading.  Fulvestrant injection is often used alone or in combination with other medications to treat advanced breast cancer or breast cancer that has spread to other parts of the body in women who have gone through menopause and have not been treated with an anti-estrogen medication like tamoxifen.
Fulvestrant injection is often used alone or in combination with other medications to treat advanced breast cancer or breast cancer that has spread to other parts of the body in women who have gone through menopause and have not been treated with an anti-estrogen medication like tamoxifen.  Bendamustine injection is used to treat chronic lymphocytic leukaemia (CLL) (CLL; a type of cancer of the white blood cells). It is also used to treat a kind of slow-spreading non-Hodgkins lymphoma (NHL: cancer that starts in a type of white blood cell that ordinarily fights infection) that has worsened during or after therapy with another drug. This injection can be used alone as well as in conjunction with other medications as part of a chemotherapy treatment plan. It works by eliminating existing cancer cells and stopping new cancer cells from growing.
Bendamustine injection is used to treat chronic lymphocytic leukaemia (CLL) (CLL; a type of cancer of the white blood cells). It is also used to treat a kind of slow-spreading non-Hodgkins lymphoma (NHL: cancer that starts in a type of white blood cell that ordinarily fights infection) that has worsened during or after therapy with another drug. This injection can be used alone as well as in conjunction with other medications as part of a chemotherapy treatment plan. It works by eliminating existing cancer cells and stopping new cancer cells from growing.  Cetuximab Injection is used to treat a kind of head and neck cancer that has progressed to neighbouring tissues or other sections of the body. It is also used to treat a form of colon (large intestine) or rectum cancer that has progressed to other parts of the body, either alone or in conjunction with other drugs. It helps to slow down or prevent cancer cell proliferation.
Cetuximab Injection is used to treat a kind of head and neck cancer that has progressed to neighbouring tissues or other sections of the body. It is also used to treat a form of colon (large intestine) or rectum cancer that has progressed to other parts of the body, either alone or in conjunction with other drugs. It helps to slow down or prevent cancer cell proliferation.  It is used in the treatment of chronic lymphocytic leukaemia (CLL; a form of white blood cell cancer) in individuals who have failed to improve after receiving at least one other treatment. Fludarabine injection belongs to the purine analogues class of drugs. It works by reducing or preventing cancer cell development in the body.
It is used in the treatment of chronic lymphocytic leukaemia (CLL; a form of white blood cell cancer) in individuals who have failed to improve after receiving at least one other treatment. Fludarabine injection belongs to the purine analogues class of drugs. It works by reducing or preventing cancer cell development in the body.  Trabectedin Injection is used in the treatment of liposarcoma (fat cell cancer) or leiomyosarcoma (smooth muscle cancer) that has migrated to other areas of the body and cannot be cured with surgery in persons who have already received specific chemotherapy drugs. It works by reducing or preventing cancer cell development in the body.
Trabectedin Injection is used in the treatment of liposarcoma (fat cell cancer) or leiomyosarcoma (smooth muscle cancer) that has migrated to other areas of the body and cannot be cured with surgery in persons who have already received specific chemotherapy drugs. It works by reducing or preventing cancer cell development in the body.  Procarbazine Capsule is used in the treatment of Hodgkin’s disease, commonly known as Hodgkin’s lymphoma. It functions by preventing the creation of proteins, RNA, and DNA, which is helpful in halting the expansion of cancer cells within the body.
Procarbazine Capsule is used in the treatment of Hodgkin’s disease, commonly known as Hodgkin’s lymphoma. It functions by preventing the creation of proteins, RNA, and DNA, which is helpful in halting the expansion of cancer cells within the body.  Gefitinib Tablets is a non-steroidal anti-inflammatory drug (NSAID) that is used to treat cell lung cancer. It is a type of anticancer medicines that prevents cancer cells from growing and spreading in the body. It’s utilised in people who have cancer that’s progressed to other parts of their bodies, have faulty epidermal growth factor receptor (EGFR) genes, and haven’t had previous cancer treatment.
Gefitinib Tablets is a non-steroidal anti-inflammatory drug (NSAID) that is used to treat cell lung cancer. It is a type of anticancer medicines that prevents cancer cells from growing and spreading in the body. It’s utilised in people who have cancer that’s progressed to other parts of their bodies, have faulty epidermal growth factor receptor (EGFR) genes, and haven’t had previous cancer treatment. 